The normal healthy vagina is an incredible ecosystem that includes diverse communities of various micro-organisms. Hundreds of species and families of vaginal flora have been identified in recent years and research is still in its early stages.
The vaginal flora is made up of different dominant types of bacteria (such as lactobacillus), fungi, and viral entities that all play an important role in maintaining the healthy functioning of the “vaginal microbiome”.
Normal (cervical and vaginal) secretions keep our vaginas clean, moist and welcoming to sperm at certain times of the month. Vaginal secretions help maintain a slightly acidic pH environment, in the range between 3.8 and 4.5. Healthy vaginal pH helps inhibit and reduce the growth of yeast. This range can vary by age, during the menstrual cycle, as well as during pregnancy and menopause.
Lactobacilli help to keep the vagina healthy by producing lactic acid, hydrogen peroxide, and other substances that inhibit the growth of yeast and other unwanted organisms. This mildly acidic environment helps protect against infection. So do the other substances they produce. Dozens of families of bacteria also play an important part in maintaining a healthy vaginal ecosystem.
There are different theories about the candida/yeast infection phenomena and the intricate interplay between the microbiota in the vaginal ecosystem. The most commonly accepted and evidence-based theory maintains that C. Albicans (Candida Albicans) is a fungus (one of many) that colonizes the vaginas of about 20 percent of women and 30 percent of pregnant women. While this “colonization” doesn’t cause symptoms, symptomatic yeast infections can develop when the balance of microbial communities within the vagina (and the gut) gets thrown off balance by medications (antibiotics, hormonal birth control, spermicides), hormonal changes (pregnancy, diabetes), poor diet (too many carbs and sugars), prolonged stress, insufficient sleep, weakened immune system and the use/overuse of feminine hygiene products.
Regarding hormones, although still controversial, studies show that while hormonal birth control does not directly harm the microbiota in the vagina, and can actually reduce the prevalence of BV (bacterial vaginosis) it does promote yeast colonization in healthy women. The synthetic hormones in hormonal birth control can increase your susceptibility to developing a yeast infection.

In my experience, working with nearly 3,000 clients who learn to identify their infertile and fertile secretions (read: normal and healthy) during the menstrual cycle, a sizable number experience other, unusual secretions (read: abnormal and unhealthy).
Going off hormonal birth control often resolves the issue (together with vaginal dryness, sexual pain, mood swings, and more). When a person learns to recognize their normal, healthy secretions, it becomes very easy and obvious to recognize unfamiliar secretions.
When our natural secretions change in color, smell, and sensation, this could be a sign of infection. Unhealthy secretions are those that cause vaginal itching, burning, soreness, redness, discomfort during intercourse, a cottage-cheesy looking discharge with a mild yeast smell (although not everyone with candida overgrowth sees a distinct discharge, and if they do, the discharge can also be watery and odorless).
Vaginal yeast infections are typically caused by an overgrowth of a fungus that lives naturally in the vagina. Candida albicans can cause an imbalance that triggers inflammation and the symptoms just mentioned.
There are two primary, common types of candida infections. In the first type, infections are very infrequent (even once in a lifetime) they occur less than once a year or once in five years. When caught early, these infections can be nipped in the bud with either traditional medications or with natural remedies. Physicians typically prescribe antifungal medications which come in different forms: creams, ointments, tablets, and suppositories. Common brands that do not require a prescription are: Miconazole (Monistat), tioconazole (Vagistat), and clotrimazole (Gyne-Lotrimin). Another common prescription-only medication is Diflucan (fluconazole).
With the second type, the infection is persistent and more frequent. It comes and goes and does not completely resolve. As a result, it can take months and even years to cure because the problem lingers, undiagnosed and untreated, on many levels, for a prolonged period. This enables the candida to spread and affect other parts of the body. This type of infection requires a more serious and rigorous approach.
For the severe cases that do not respond to the usual anti-fungal medications, physicians will resort to more extreme treatments like boric acid or sulfa-based antibiotics (super drugs) like sulfonamide and fluconazole (Diflucan). If someone in this situation truly wants to heal, naturally, there is another way; it involves a lifestyle make-over. Excellent results can be achieved by working with an experienced naturopath who will prescribe a very specific diet (for up to six months on average), together with herbal formulas and supplements. Working with a body-mind practitioner can also lead to long-term healing and recovery.
The importance of diagnosing a candida or yeast infection cannot be understated. Many women self-diagnose and many others will be given a prescription by their gynecologist who doesn’t bother to perform a proper vaginal culture.
Note: If you experience symptoms for the first time, get checked by your gynecologist and insist on a vaginal culture. Sometimes other strains of candida will be resistant to the medication you are given. Sometimes, a bacterial infection can coincide together with a fungal infection so a culture is necessary to accurately diagnose and treat the full situation. And perhaps most importantly, if someone is not having safe sex or sex with multiple partners- what one thinks is just a yeast infection could in fact be a symptom of a sexually-transmitted infection. In other words: No one should use anti-fungal medications without a proper diagnosis.
For those seeking non-pharmaceutical solutions to their occasional yeast infection, the following remedies can be tried. Many are anecdotal and many swear by them, but most have not been fully researched or been found to be effective. It is best to begin a treatment regimen with an experienced practitioner who can guide you in how to use these substances, in what doses, and for how long a time. One can find recipes on the internet but try to confirm that the source of information is professional and reliable.
If you are prone to yeast infections or want to ward them off before they cause havoc, follow these suggestions:
Sit quietly and close your eyes. Take five deep breaths and be aware of how you follow your breath – for three minutes. Then meditate, observe yourself, in a non-judgmental way, while asking yourself this question: “If my vagina could talk, what would it say”? Ask your vagina why it is giving you such a hard time. Ask your symptoms, “Why are you here and what do you want from me?” Connecting to your intuitive self and subconscious can allow thoughts, ideas, and associations to surface which can surprise. Often, unhealthy relationship dynamics will manifest themselves through “sexual” symptoms. I have known countless women who have healed from chronic candida who can confirm this body-mind connection.
La-bruit. To your health.
Accreditation recognized by The Association of Fertility Awareness Professionals
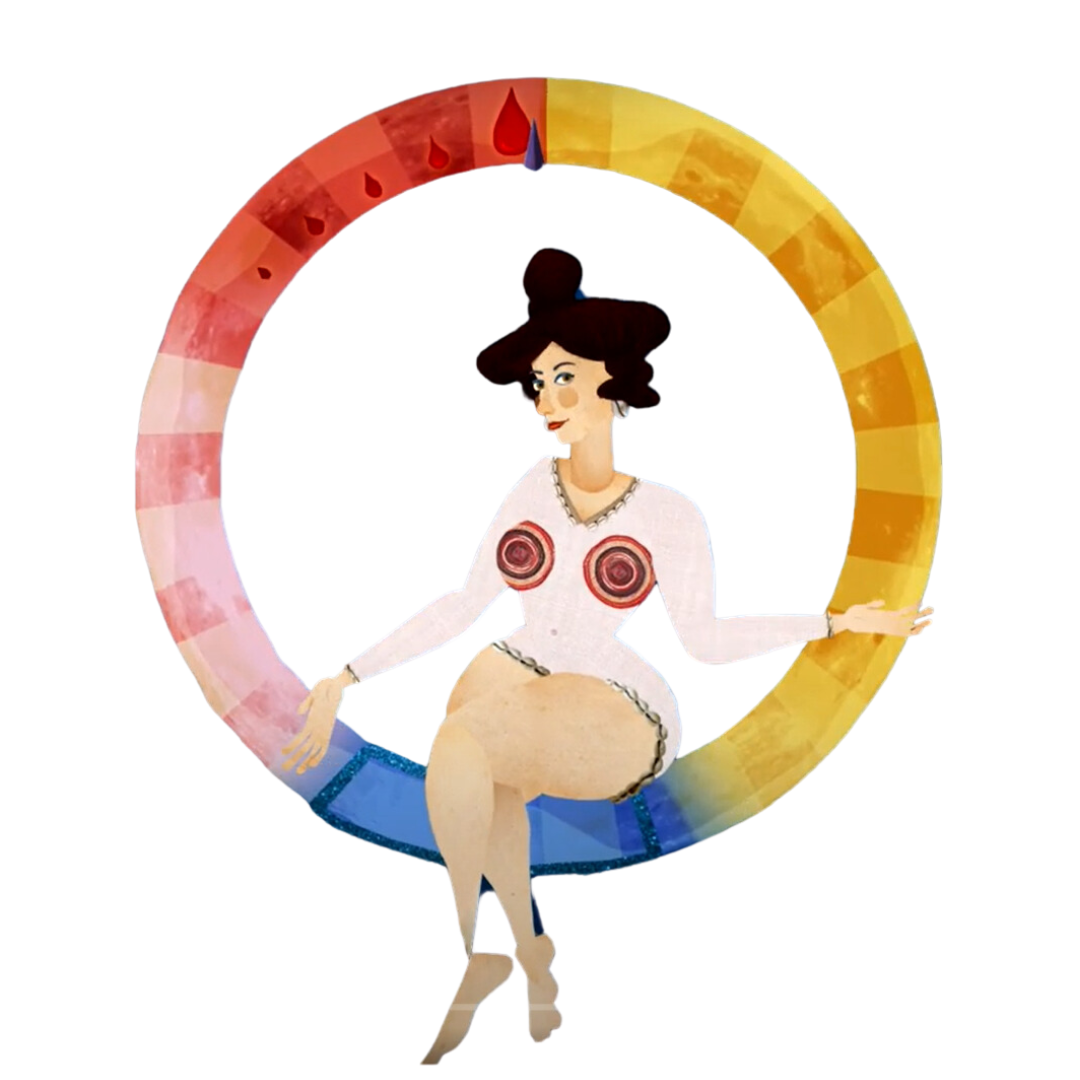
* All illustrated characters are taken from “The Monthly Cycle,” a short film by Ada Ramon and Ofek Shamir.
Quick Links
The information presented on the site is for educational purposes only and is not intended to replace medical advice from a qualified doctor or other health professional. For convenience, the information is written in the feminine form, but refers to anyone born with a uterus and ovaries, including those who do not identify as women
Contact Me
Join Our Newsletter