I DEFINING BASIC TERMS
Efficacy is a complex term that is widely misunderstood and misrepresented. It requires translation, nuance, and knowledge about basic terms so users can make informed decisions about contraception.
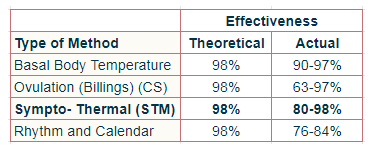
All birth control methods have two kinds of effectiveness rates: theoretical/ method effectiveness and actual/user effectiveness.
Method effectiveness refers to the degree of efficacy reached under ideal conditions when used correctly and consistently by the individual/couple. All contraceptive methods have a theoretical effectiveness of 98% or higher. Method effectiveness is another way of stating “perfect use”.
User effectiveness refers to the degree of efficacy reached under typical, real-life conditions, taking into account human nature, which is often less than perfect, and even irrational. User effectiveness is another way of stating ‘imperfect use.”
One way to grasp the practical significance of perfect vs imperfect use is by dividing all methods into four basic sub-types; each type of method requires a different mindset, priority, value and skill set. There are methods that require:
- no behavioral effort on the part of user e.g. IUDs and implants
- low level of behavioral effort, e.g. hormonal methods which require remembering to take a pill every day or replacing a vaginal ring every month
- medium level of effort, e.g. barrier methods like diaphragms and condoms, spermicides and withdrawal
- high level of effort, e.g. FAM/STMs which are 100% user-controlled
As a rule, hormonal methods and IUD’s have higher efficacy whereas most non-hormonal methods generally have lower efficacy. Why? Because they require more skill, diligence, and long-term effort. As a result, there can be a 10-20% gap between perfect use and typical use. For example, hormonal methods have a nearly 100% theoretical effectiveness rate (when used perfectly- correctly and consistently) but actual effectiveness is closer to 90%, because they are not used perfectly (most surveys reveal that at least once a month, users forget to take their pills at the right time).
In theory, all methods are inherently reliable, but in reality, they can be less than reliable because not all people are consistently diligent and responsible when implementing them. As a rate, theoretical effectiveness refers to perfect users -those who follow the rules every time and don’t take risks or chances. Actual effectiveness includes those who are perfect users and those who are not.
So here is a list of things you will want to know:
II APPLYING BASIC TERMS
- A researcher cannot accurately measure “perfect use” because s/he is not present during any sexual act in order to determine whether or not a couple is using a given method in a correct and consistent way. Because of this methodological pitfall, researchers rely on another measure: failure rate. They will ask the question not in terms of perfect use but in terms of typical use or user failure. In other words, how many people experience an unintended pregnancy while using a given method of contraception during a certain period of time under study?
- Birth control effectiveness rates/statistics published by reproductive/ health organizations (e.g. CDC, WHO, Contraceptive Technology, Planned Parenthood) are actually “estimates” based on a mixture of data collected from clinical trials and large population surveys like the National Survey of Family Growth (NSFG). They are not true, absolute numbers derived from exact circumstances nor are they numbers that personally apply to you. Researchers use various mathematical formulas to calculate these estimates, because this is the next best way to estimate efficacy.
- An effectiveness rate deemed high in one study population, among one ethnic/religious group which values and practices abstinence during fertile days cannot be expected to reach the same efficacy among secular folks with different values who live in another culture. This means that efficacy rates from one study are not universal and so they cannot be applied to other populations. For example, measuring the efficacy of condom use among adults in Japan (a country and culture which takes condom use very seriously and strictly) will yield a much higher efficacy rate than among a population of teenagers in the U.S.). The efficacy of birth control pills among adolescents is naturally lower than it is for older people. These factors enable us to understand that the “technical” and inherent factors which determine effectiveness are not the bottom-line. Culture, religious beliefs, age, behavior, maturity, partner support and values have a direct effect on the statistical efficacy reached by an individual user/couple.
III HOW EFFECTIVE IS FAM (AND OTHER STMs)?
This depends on how the method is used and how “strict” a couple decides to be, particularly during the fertile days of the cycle. FAM, as taught by Poriutivit (a variation of the book, TCOYF), is one of a dozen schools or variations of the “Sympto-Thermal Method” (STM’s). STMs rely on observing and interpreting at least two (out of three) primary fertility signs during the menstrual cycle: basal temperature (thermal), cervical secretions ( a sign/symptom of ovulation) and cervical position (recommended though not mandatory). Poriutivit is a double-check method which requires the use of two indicators for determining when the window of fertility opens and two indicators for when it closes. Poriutivit may be more effective than other STMs because it requires internal secretion checks in certain circumstances.
All STM variations are based on the same science, but lean on different research studies and ideological approaches. They have the same goal: giving users tools for identifying the fertile days of the cycle and teaching the rules that “protect” the user from unintended pregnancy. Some STM programs are funded and promoted by the Catholic Church and encourage abstinence-only during the fertile days and other STM’s are promoted by secular groups who encourage couples to make their own choices regarding the use of barrier and other methods during the fertile days.
STMs are very effective among perfect users. Among imperfect users, they can be very “unforgiving.” On average, typical users (self- taught) can experience a 20% or higher failure rate during the first year of use. Among perfect users (taught and followed with a certified teacher), first-year failure rates are under 5%. For couples who only have intercourse after ovulation or who correctly use two methods simultaneously during the fertile days, user effectiveness can approach 100% (re the latter, we do not yet have high-quality studies to confirm this). Just remember that a “number” does not protect you; correct and consistent use does.
Unlike hormonal and IUD methods, STM’s like FAM have a relatively wider range of effectiveness because:
- they are user-dependent and require personal involvement and responsibility
- they are more challenging to research (perfect use with natural methods involves more than remembering to swallow a pill every day) and
- they involve time, standardized learning, follow-up during learning phase and often require supervision/follow-up by a qualified teacher.
- they require communication skills, partner cooperation, high motivation, on-going decision-making and discipline
- their success depends on the right sync between personal values and lifestyle factors as well as commitment and motivation to monitor one’s biomarkers (fertility signs)
Unlike conventional methods of contraception, STM’s (including Poriutivit) divide the menstrual cycle into 3 phases of fertile and infertile days:
Phase 1: from first day of menstrual bleeding until fertile window opens (lower risk)
Phase 2: all the days of the fertile window (typically 3-5 on average) (highest risk)
Phase 3: from time fertile window closes (based on two signs) to the next period (typically 10-14 days on average) (no risk)
Since each phase confers a different risk, effective use of FAM requires that:
- Users always use one barrier/back-up method (during learning phase) during Phase I and two barrier/back-up methods during the fertile days in Phase 2.
- Users knows how to identify the fertile days/window of the menstrual cycle and then adapt their sexual behavior to the method rules, as taught.
- Users properly chart BBT & secretion changes for confirming the opening and closing of the fertile window. Without a clear, defined window, there is no method.
- Users acquire experience, skill and confidence with other back-up methods (condoms, withdrawal, diaphragms, spermicides) before they start to use them in “real time.” Since no back-up method is 100% effective when used alone, we combine two methods simultaneously to increase effectiveness, e.g. a spermicide used together with a condom; withdrawal with the sponge, or a diaphragms with gel. This requirement is best understood by the common example: If and when a condom breaks on a fertile day, the result can be a 100% pregnancy. Therefore we need another method to increase efficacy.
- Couples remember that FAM is not a “stand-alone” method. When first developed, it assumed that couples would abstain for nearly half or more of the days of the cycle. If a couple chooses to use other methods during fertile or potentially fertile days, then the effectiveness of these other methods supersedes the effectiveness of FAM/STMs (which are typically based on abstinence-only).
- Couple understands the difference between method failure and user failure.
IV WHEN FAM IS “UNFORGIVING”
Unintended pregnancies are almost always the result of user failure, which occurs when users are self-taught, chart inconsistently, have trouble identifying the fertile window, err in interpreting their charts, ignore or incorrectly use method rules, or engage in risk-taking behavior during the pre-fertile and fertile phase, i.e. engaging in unprotected or partially protected sex. And while a user will become more proficient and knowledgeable about her cycle over time, she can also become complacent over time, by assuming she knows what is/is going to happen, based on past cycles/charts (“auto-pilot mode). These “errors” are less likely to occur when learning FAM from a certified, experienced instructor, particularly during the learning phase (typically 3 months or cycles). This is particularly relevant when a new learner is in hormonal transition e.g. coming off hormones, post miscarriage or abortion, breastfeeding, or in peri-menopause.
V FAM EFFECTIVENESS
- A literature review of some FABMs and STMs shows a range of effectiveness.
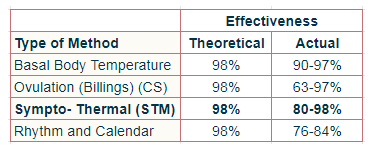
2. In theory, all methods are highly effective whereas actual, user effectiveness shows a wider range of efficacy. It provides a clue as to how subjectively easy or difficult a method will be to use. For example, the Ovulation (Billings) Method may require more experience and expertise than the Temperature Method alone because interpreting (subjective) changes in secretions is more complex than interpreting (objective) changes in basal temperature. Observational methods are inherently more precise because they require daily monitoring in the present, whereas calculation methods are generally less precise because they rely on past cycle lengths alone.
- Some STMs have rules which prohibit intercourse until the fertile window closes; this means limited days of sexual freedom and fewer days of “potential risk, ” which translates into a higher effectiveness rate. Other STMs have rules which incorporate individual choice so users can decide if and how to protect themselves during the pre-fertile and fertile days.
- If/when a couple uses other methods, the effectiveness of these other methods replaces FAM. When back-up methods are used incorrectly or inconsistently, then the risk of unintended pregnancy increases.
- Most STM’s teach that any secretion (even dry, sticky, acidic) observed after menstrual bleeding and staining is potentially fertile. Poriutivit believes that users can learn to recognize infertile secretions both before and after ovulation, just like during prolonged periods of breastfeeding. Since new learners need time and experience to understand their individual secretion pattern, they must adhere to strict rules while charting their first 4-6 cycles. After a supervised learning period, users can choose to shift from “more strict” to “less strict” rules, or short-cuts. A high level of skill, diligence, confidence and responsibility is necessary for couples wanting to maximize their days of “sexual freedom”.
- The bottom line is this:
Personal, statistical, actual effectiveness for FAM (and other STM’s) is highly dependent on the characteristics of the user/s, i.e.
- Knowing and understanding how the method works
- motivation to prevent pregnancy + satisfaction with the method
- correct and consistent use
- skill, experience, confidence
- partner support/cooperation and social support/acceptance
- receiving follow-up from a qualified teacher
- the hormonal health and overall health of the user
- the ability to correctly identify the fertile window and use two simultaneously methods on those days
TAKE-HOME MANTRAS
- There is no perfect method or method that is 100% (only abstinence).
- A number (statistic) does not protect you against unintended pregnancy; correct and consistent use of a method protects you.
- Technology can fail people just as people can fail technology.
- Contraceptives are imperfect and can fail the most diligent users.
- Using two methods together dramatically lowers the risk of accidental pregnancy.
- FAM works best when it syncs with personal values, priorities and lifestyle.
- FAM works when chosen for the right reason: it’s the best method for someone’s values, lifestyle, health and sexual relationship. Choosing FAM as the “default” method (because all other methods are rejected or unacceptable) is a different, “weaker” choice as it may not confer high efficacy over time.
- FAM is not for everyone. It works best when there’s a genuine desire to know your body and take full responsibility for your sexual health. It requires a commitment to learn properly and having a supportive partner. When chosen for the right reasons, FAM can be a highly effective and safe method of contraception.
REFERENCES
Rates calculated from studies reviewed in:
-
- Contraceptive Technology, Robert Hatcher, et al.18th Revised Edition, 2004, pp 221-252.
- Contraceptive Efficacy, J. Trussell. Global Library Women’s Medicine (GLOWN), 2014
- Contraceptive Failure in the United States: Estimates from the 2006–2010 National Survey of Family Growth, A. Sundaram et al. 2017